
27th June, 2025
Health Care
When someone you love is admitted to the Intensive Care Unit (ICU), it can feel like the ground has shifted beneath you. Worry, fear, and confusion often follow. If you're in this situation, knowing what the ICU is, what kind of care it offers, and how to stay connected with ...
Read More
5th June, 2025
Health Care
Irritable Bowel Syndrome (IBS) is a common digestive disorder that affects many people worldwide. Understanding the causes, symptoms and management strategies for IBS can help those who live with the condition improve their quality of life. Here, we share some of the causes, symptoms and management methods for IBS.What ...
Read More
29th May, 2025
Health Care
A general surgeon performs a broad range of surgeries involving the abdominal organs, digestive tract, soft tissues, hernias, and thyroid. In Kolkata, many hospitals offer general surgical services, but the skill and experience of each surgeon can vary. A general surgeon handles both elective and emergency cases and may also ...
Read More
22nd May, 2025
Health Care
Diabetes has become one of the most common chronic conditions in India. With millions affected, the need for timely and effective care has never been more crucial. A key step in managing diabetes involves finding the right doctor. Whether you have Type 1, Type 2, or gestational diabetes, the right medical guidance ...
Read More
15th May, 2025
Health Care
Peerless Hospital has firmly established itself as one of the leading hospitals in Kolkata and Eastern India. This reputation is supported by numerous accreditations and awards that highlight the hospital's commitment to quality and excellence in healthcare.In 2024, Peerless Hospital earned multiple distinctions at the ICC National Healthcare Excellence Awards, ...
Read More
6th May, 2025
Health Care
Every year, on the first Tuesday of May, World Asthma Day is celebrated. This year it is being celebrated on 6th May.The theme for World Asthma Day 2025 is "Make Inhaled Treatments Accessible for All"The day helps raise awareness about this common respiratory condition. Asthma or bronchial asthma is ...
Read More
30th April, 2025
Health Care
Cervical cancer is one of the most preventable types of cancer, yet it remains a major health concern for women worldwide. The key to beating it is awareness-understanding the risk factors and spotting early symptoms can make all the difference. In this blog, we'll break down everything you need to ...
Read More
24th April, 2025
Health Care
Coronary artery bypass grafting (CABG) is a procedure that is used to treat coronary artery blockages. The life saving treatment can help blood flow normally to the heart, which might have been disrupted because of the blockage. Previously, such a surgery would involve opening the chest by making a large ...
Read More
17th April, 2025
Health Care
The relationship between the liver and the digestive system is more interconnected than many realize. This connection, known as the gut-liver axis, plays a critical role in maintaining overall health. Understanding how the gut and liver interact can help in managing digestive health and preventing liver diseases. Here, we share ...
Read More
10th April, 2025
Health Care
Mental health care is as vital as physical health care, yet it often goes overlooked, misunderstood, or stigmatised. Whether you experience stress, anxiety, depression, or more serious mental health conditions, seeking support from a trusted psychiatrist can significantly improve your quality of life. For residents of Kolkata, finding the right ...
Read More
3rd April, 2025
Health Care
A healthy digestive system is essential for maintaining overall health, yet many overlook gastrointestinal issues. These problems often signal underlying conditions that demand specialised care. Gastroenterology specialists, who are experts in digestive health, play a crucial role in diagnosing and treating these conditions. Recognising the signs that require medical attention ...
Read More
27th March, 2025
Health Care
Neck surgery is a significant procedure that requires careful post-operative care. Recovery can be a gradual process, but understanding the typical timeline and following essential tips can help you return to your normal activities safely and efficiently. Here, we share the timeline and some tips about recovery after a neck ...
Read More
20th March, 2025
Health Care
Minimally invasive cardiac surgery is a revolutionary approach to heart surgery that offers patients a safer and less traumatic alternative to traditional open-heart surgery. This technique involves smaller incisions, reduced blood loss, quicker recovery times and less postoperative pain. It is particularly advantageous in certain cases where traditional surgery may ...
Read More
13th March, 2025
Health Care
Accidents can happen unexpectedly at any time. Knowing how to act in these situations is very important, as it helps reduce injuries and ensures the safety of everyone involved. While different accidents may need specific actions, there are some general steps you can follow in most cases. In this blog, ...
Read More
6th March, 2025
Health Care
Ear, nose and throat (ENT) infections are some of the most frequent health issues in children. These infections can cause significant discomfort and, if left untreated, may lead to complications. Understanding the common types of ENT infections, their symptoms and when to seek medical care is vital for parents and ...
Read More
27th February, 2025
Health Care
Knee replacement is a major surgery that requires considerable preparation, both physically and mentally. Even after the surgery is complete, you will need to adjust your lifestyle and slowly adapt to using the prosthetic knee. Here, we share a step-by-step guide about some of the preparations that you should take ...
Read More
21st February, 2025
Health Care
Angiography is an imaging technique that is often used to diagnose a mechanical block in the coronary artery of the heart. If indeed a mechanical block is found, it needs to be opened if it's a major block (more than 70%). If no mechanical block is found one can relax and ...
Read More
13th February, 2025
Health Care
You would need to seek the help of orthopaedic specialists if you suffer from musculoskeletal disorders. So, if you have issues with your bones, tendons, ligaments or muscles, these medical experts can get to the bottom of the condition and develop a care plan. But, before you head to them, ...
Read More
6th February, 2025
Health Care
Kidneys are an important part of the urinary system. They remove waste products from blood, maintain fluid balance, and regulate electrolyte concentrations within the body. In addition to filtering bodily fluids, the kidneys play a crucial role in regulating blood pressure by secreting hormones that help keep electrolytes and fluid ...
Read More
30th January, 2025
Health Care
The primary cause of anaemia in pregnant women is the lack of necessary iron levels in the body. Iron is an essential element when producing red blood cells. Other factors can lead to pregnant women developing anaemia, such as poor absorption of iron, multiple pregnancies, inadequate dietary intake and certain ...
Read More
23rd January, 2025
Health Care
Cardiac emergencies, especially heart attacks, can strike suddenly without warning. If someone you know experiences cardiac arrest, acting quickly is critical for their survival. Providing first aid while waiting for medical help can significantly increase their chances of a positive outcome. Here's what you can do:Be aware of the ...
Read More
16th January, 2025
Health Care
Thalassemia disease is a type of genetic blood disorder that leads to abnormal hemoglobin production. This causes a reduction in red blood cell (RBC) count and oxygen-carrying capacity. Thalassemia is inherited, which means it is passed down from parents to children. This inheritance pattern results in the body's inability to ...
Read More
19th December, 2024
Health Care
Keeping your child safe is not just important when they are awake. The same protection has to be given to them even when they are asleep. Creating a safe and secure sleeping environment involves several considerations. Here, we share some useful insights about creating a safe sleeping environment for your ...
Read More
12th December, 2024
Health Care
Prostate cancer varies from low-risk indolent tumors to fast-progressing tumors leading to life-threatening conditions if not diagnosed and treated appropriately. A significant obstacle in delivering effective treatment is the abundance of misinformation about the disease, its symptoms, and treatments. Here, we address and debunk some prevalent myths related to prostate ...
Read More
5th December, 2024
Health Care
The prognosis for breast cancer is significantly improved when the disease is identified early on. Recognizing the key symptoms associated with breast cancer is important, as it empowers individuals to seek timely medical intervention which significantly improves the chances of successful treatment. Here, we share the common signs and symptoms ...
Read More
28th November, 2024
Health Care
Breast cancer is a serious health condition where early detection and swift medical intervention are key to saving lives. However, several myths about breast cancer persist, which can prevent timely treatment and worsen the condition. Here are some of the most common myths about breast cancer debunked:Myth: Men cannot ...
Read More
21st November, 2024
Health Care
Prostate cancer is a significant health concern for men worldwide. This disease occurs when cells in the prostate gland, a small but crucial part of the male reproductive system, grow uncontrollably. This guide delves into various aspects of prostate cancer, including its symptoms, risk factors, diagnosis, treatment options, prevention strategies, ...
Read More
7th November, 2024
Health Care
Thyroid problems can cause a wide range of symptoms, which can affect your bones, muscles and heart. The thyroid gland releases T3 and T4 hormones, which are highly important for the maintenance of proper bodily metabolism, energy, and temperature. You must understand the functionalities of the thyroid gland in detail ...
Read More
19th September, 2024
Health Care
Breast cancer is a common condition affecting women, and rarely, men. While age remains the most significant factor, many other aspects can influence your individual risk. Recognizing these factors empowers you to make informed choices and potentially detect the disease early on. Here's a breakdown of some key risk factors:...
Read More
13th September, 2024
Health Care
Falls among the elderly pose a significant concern, often leading to severe injuries or increased health risks. With age, individuals experience various physical changes and may face health conditions or take medications that elevate their risk of falling. Despite these challenges, seniors can implement numerous strategies to minimise their risk ...
Read More
26th August, 2024
Health Care
Gynaecological cancers refer to cancers that develop in the reproductive organs of women, including the ovaries, uterus, cervix, vulva, and vagina. These cancers can be very serious, and early detection is critical to effective treatment and a positive outcome. Gynaecological cancers are relatively common, and every year, thousands of women ...
Read More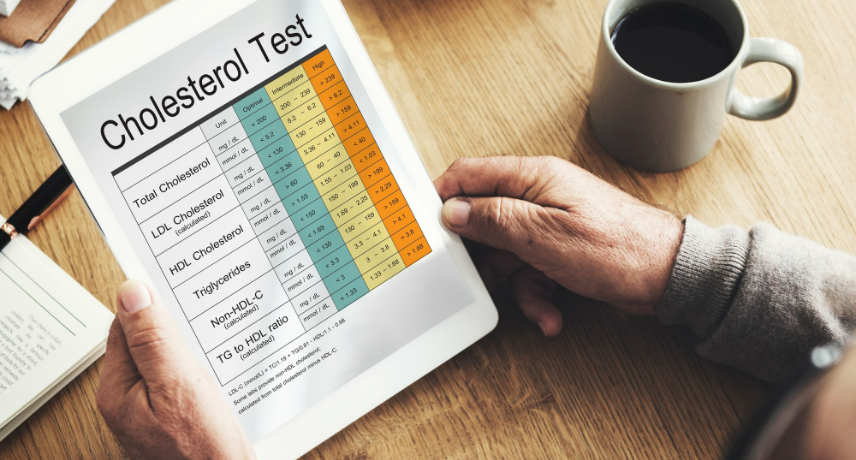
22nd August, 2024
Health Care
Hyperlipidemia or high cholesterol, means you have too many lipids (fats) in your blood. Your liver metabolizes cholesterol to help you digest food and makes hormones from it. Since your liver can make as much cholesterol as you need, the cholesterol in your food is extra.Normal cholesterol is below 200 ...
Read More
9th August, 2024
Health Care
Maintaining overall bone health is important, because the bones provide support and structure to our bodies and protect internal organs. However, as people age, they lose bone mass and risk developing osteoporosis. Osteoporosis is a common disease that causes bones to become weak and brittle. People can take proactive steps ...
Read More
18th July, 2024
Health Care
4 out of a 100 Indians run the risk of being afflicted with colorectal cancer in their lifetime. The good news is that advancements in medical science now ensure that if detected at an early stage, the ailment is completely curable. Naturally, early detection is the key. However, the incidence of those ...
Read More
11th July, 2024
Health Care
A pressure injury, formerly known as a pressure ulcer or bedsore, occurs when different kinds of forces are applied to the body, resulting from prolonged pressure on the skin and underlying tissues. They mostly form in regions with bony structures beneath the skin, such as the hips, buttocks, head, ankles, ...
Read More
19th June, 2024
Health Care
Parents always try to protect their children from accidental injuries. However, this can be a difficult task, especially when the children are still young and they miscalculate the risk involved with the way they play or move. Since such accidents can happen at any time, parents have to take proactive ...
Read More
12th June, 2024
Health Care
Ovarian cancer is often known as a silent killer. This is because the disease does not show any major symptoms in its initial stages, making diagnoses challenging. By the time ovarian cancer is generally detected, it progresses to an advanced stage and can put the patient's life in substantial risk. ...
Read More5th June, 2024
Health Care
Cardiac health check-ups are important procedures that can help one stay updated about their heart's current condition. Some individuals are more likely to suffer from these kinds of diseases. Factors, such as family history, obesity, age, smoking habits and several others can play a vital role in determining whether one ...
Read More
29th May, 2024
Health Care
Proper emergency medical services/care can mean the difference between life and death. Swift access to specialized care, a skilled medical team, and well-equipped facilities can significantly increase the chances of survival and recovery. To help you understand more about medical emergency services, we share with you some of the ...
Read More
23rd May, 2024
Health Care
Childhood days are the most memorable part of each one of our lives. I am sure everyone will agree to this fact. As we all know, most children are somewhat mischievous. Their daily activity includes running around, playing games and doing naughty stuff. While doing so they too get hurt ...
Read More
8th April, 2023
Health Care
Health check ups are important at all stages of life. Regular check ups are needed to diagnose any condition at an early stage or simply to control existing conditions. For senior citizens, health check ups are done to evaluate and monitor their overall health and well-being. Here is a list ...
Read More
6th May, 2023
Health Care
Common health problems in elderly women and how to manage them right: useful insights be one of the best hospitals in kolkata.Ageing is a natural process that can lead to a range of health problems, especially in elderly women. These health issues can significantly impact the quality of life ...
Read More
30th November, 2023
Health Care
Cancer is caused by a combination of genetic, environmental and lifestyle factors. It can affect anyone, regardless of age and gender. However, there are certain types of cancer that affect women more than men. In this article, we will discuss some of the common types of tests that detect cancer ...
Read More
18th June, 2021
Health Care
The pregnancy period is normally a joyous, fulfilling and satisfying experience for most mothers and their families usually culminating in the safe delivery of a healthy baby marking the beginning of a new era in the family timeline. However, the going is not entirely smooth in every case and complications ...
Read More
18th June, 2023
Health Care
Tobacco smoking is the act of burning tobacco and inhaling the resulting smoke, which then enters the bloodstream. Approximately 23 percent of the global population engages in cigarette smoking. When it comes to smoking side effects, numerous studies have established a strong association between tobacco smoking and various serious health conditions, ...
Read More
23rd June, 2023
Health Care
All chest pains are not heart attacks and all heart attacks may not be associated with chest pain.In today's society, heart attacks have become alarmingly prevalent due to the sedentary lifestyles and the overconsumption of foods high in saturated fats. These factors have contributed to a significant increase in ...
Read More